Past Issues
Hypocalcemia-induced Camel-hump T-wave, Tee-Pee sign, and Bradycardia in a Car-painter of a Complexed Dilemma: A Case Report
Yasser Mohammed Hassanain Elsayed
Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
Corresponding author: Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt, E-mail: [email protected] Received : September 04, 2020 Published : September 29, 2020
ABSTRACT
Rationale: Electrocardiographic is a fundamental tool for a cardiologist, critical care physician, and emergency medicine specialist. The electrolyte imbalance is a very important entity in clinical medicine management. Camel-hump T-wave and the Tee-Pee sign, recently; Wavy triple and Wavy double signs of hypocalcemia (Yasser’s sign) are electrocardiographic findings linked to electrolyte deficiencies. Patient concerns: A middle-aged male car-painter patient presented to the emergency department with atypical severe twisting chest pain, hypocalcemia, hypokalemia, and hypernatremia. Diagnosis: Hypocalcemia-induced Camel-hump T-wave, Tee Pee sign, Wavy double sign of hypocalcemia (Yasser’s sign), and bradycardia in a car- painter. Interventions: Electrocardiography, arterial blood gases, oxygenation, and echocardiography. Lessons: The dramatic reversal of Camel-hump T-Wave, Tee-Pee sign, Wavy double sign of hypocalcemia (Yasser’s sign) after calcium gluconate injection interpret that these signs were due to hypocalcemia. The twisting chest pain and its limited disappearance immediately after calcium gluconate injection indicate the pain can be named as “chest tetany”. Non-atropine bradycardia response is evidence that the management of the cause of bradycardia sometimes is essential e.g. hypocalcemia in the current case. Outcomes: There was a dramatic response of both clinical and electrocardiography including Camel-hump T-wave, Tee Pee sign, the wavy double sign of hypocalcemia, and bradycardia.
KEYWORDS: Hypocalcemia; Camel-hump T-Wave; Tee Pee sign; Bradycardia; Car-painter; A complexed dilemma
ABBREVIATIONS
ABG: Arterial blood gases; ECG: Electrocardiogram; IHD: Ischemic heart disease; O2: Oxygen; RBBB: Right bundle branch block; VR: Ventricular rate.
INTRODUCTION
Specific and several changes because of electrolyte disturbance may be detected on an electrocardiogram (ECG) [1]. ‘Camel hump’ T-waves is an innovative expression by Amal Mattu to appointing to T-waves that have a double-peak. However, there are two causes implicated in a camel hump T-waves: Prominent U waves fused to the end of the T-wave is identified in severe potassium depletion. Hidden P-waves plunged in the T-wave more commonly detected with sinus tachycardia and all degrees of heart block [2]. Anyhow, by its name, the T-waves indicate the shape it exhibits (double-peaks). Indeed, these T-wave abnormalities may be seen in hypothermia and severe brain damage. So, it is a non-specific sign [3]. Indeed, the T-wave has two humps (like a camelback). Thus, the highest hump of both should be chosen. If the T-wave has a positive and negative hump (or the other way around), the tallest hump also should be selected (the first hump is always the highest amplitude which needs to draw the tangent) [4]. The prolongation of the QTc-interval is a non-specific ancient ECG sign for hypocalcemia [5]. However, QTC prolongation will be a risk to serious ventricular arrhythmias [6]. Wavy triple an electrocardiographic sign (Yasser Sign) is a recently a novel diagnostic sign innovated in hypocalcemia. Related wavy double an electrocardiographic sign also was prescribed in hypocalcemia which is mostly seen with either tachycardia or bradycardia [6]. The “Tee-Pee sign”, so-called as it resembles the shape of a traditional Native American Indian’s home. Johri AM, et al. found a case in which a combination of hyperkalemia, hypocalcemia, and hypomagnesemia resulted in precordial QRS-complexes with peaked T-waves, prominent U-waves, and prolongation of the descending limb of the T-wave [7]. The T-wave that interlocking the U-wave was the result that is called the “Tee-Pee Sign” due to the shape of the QRS-complexes like the conventional fashion of Native American Indians dwelling. The incorporation of prolongation of both the ST-segment and descending limb of the T-wave resulted in pseudo-prolongation of the QT-interval [7].
CASE PRESENTATION
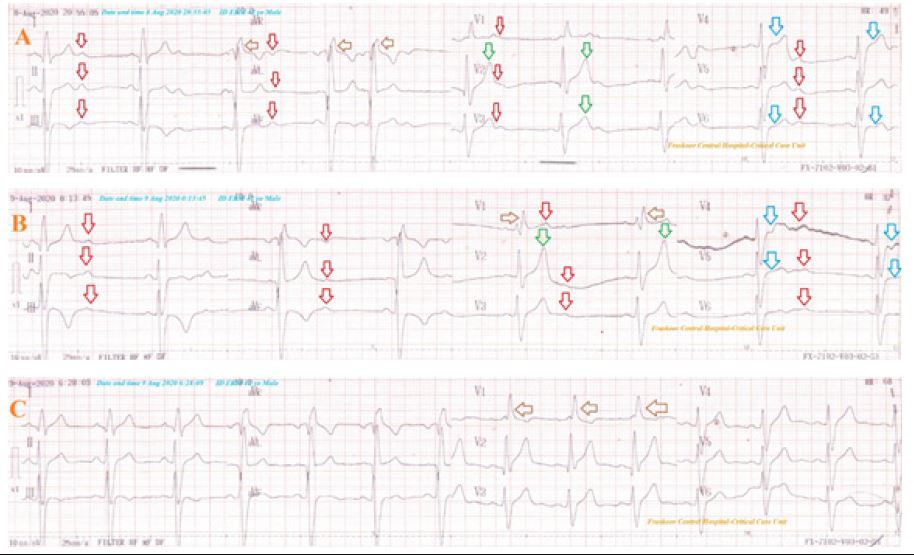
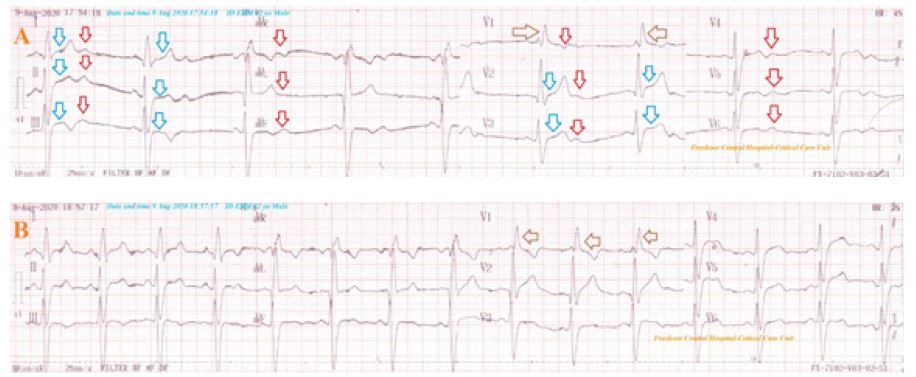
A 42-year-old married, male, car-painter, Egyptian, heavy smoker patient presented to the emergency department with acute chest pain. The chest pain was severe, twisting, radiating to the right arm, and increasing with effort. He was a heavy cigarette smoker (30-40 cigarettes per day for 19 years). The patient denied a history of cardiac or other relevant diseases. Upon examination, the patient appeared irritable, distressed, and slightly tachypneic. His vital signs were as follows: blood pressure of 130/70 mmHg, the pulse rate of 48/bpm; and regular, the respiratory rate of 22/min, the temperature of 36.6°C, and the pulse oximeter of oxygen (O2) saturation of 96%. No more relevant clinical data were noted during the clinical examination. The patient was admitted to the ICU as anginal pain with bradycardia, severe hypokalemia, and severe hypocalcemia. Urgent ECG tracing on ICU admission showed widespread “U”-waves thorough ECG, “Tee-Pee sign”, “Wavy double sign of hypocalcemia” (Yasser sign), evidence of right bundle branch block (RBBB), and sinus bradycardia of VR;48 bpm (Figure 1A). The patient was initially managed in the ICU with anti-anginal therapy. A 100% O2 inhalation using nasal cannula at the rate of 5 L/min was administered. Aspirin; four oral tablets (75 mg), clopidogrel; four oral tablets (75 mg), enoxaparin; twice SC daily (60 mg), and atorvastatin; one oral night tablet (40 mg) were urgently given. Pethidine HCL (100 mg) was given for chest pain in intermittent doses as needed. An initial dose of IV 0.5 mg atropine which was repeated to a total of 3 mg. Potassium chloride (KCl) was given by IV infusion (two 5ml ampoules of 15% KCl, containing 150 mg/ml) in one liter of dextrose 5% over 4 hours with rating 10mmol/hour. There was no response. ECG tracing was taken within 3.18 hours of A-tracing and after starting the anti-ischemic measures, IVI of Potassium therapy, and three amps of IV atropine. It nearly showed the same of A-tracing but with marked sinus bradycardia with VR; 36 bpm (Figure 1B). The immediate ABG showed compensated respiratory alkalosis (PH: 7.436 mmHg, PCO2: 32.2 mmHg, HCO3: 21.7 mmHg, and PaO2: 91 mmHg). Measured random blood sugar was 104 mg/dl. Full blood count (FBC): Hb was 12.1 g/dl, RBCs: 4.25*103/mm3, WBCs: 5.8*103/mm3 (Neutrophils: 57.3 %, Lymphocytes: 37.6%, Monocytes: 5.1%), Platelets: 99*103/mm3, SGPT: 27 U/L, SGOT: 33 U/L, serum creatinine: 0.8 mg/dl, blood urea: 28 mg/dl. Plasma sodium was s (146 mmol/L). Serum potassium was very low (2.9 mmol/L). Serum calcium showing hypocalcemia with ionized calcium; 0.43 mmol/L. The troponin test was negative (less than 2 ng/ L). Later echocardiography was normal with EF 61%. No more workup was done. Two calcium gluconate ampoules (10 ml 10% over IV over 20 minutes) were given as an emergency dose. Maintenance therapy with IVI calcium gluconate ampoules (10% with the rate; 0.5 mg/kg/hour over IV over 6 hours) was the infused. The patient was discharged within 24 hours of clinical, electrocardiographic, and laboratory improvement. ECG tracing was taken within 9.33 hours of A-tracing and immediately after 2 amp of IV calcium therapy showing nearly normalization of all above ECG findings but with still evidence of RBBB and VR: 68 bpm (Figure 1C). Serum potassium and ionized calcium after the correction was (3.45 mmol/L) and (0.76 mmol/L). Recurrence of the same initial clinical and electrocardiographic picture had happened but with absent “Tee-Pee sign” (Figure 2A). The same above calcium gluconate ampoules was repeated with above emergency dose then, with maintenance dose; 0.5 mg/kg/hour IVI over 4 hours. Nearly normalization of clinical and all above ECG findings but with still evidence of RBBB and VR; 68 bpm occurred (Figure 2B). The patient was discharged within 12 hours after controlling the chest pain, and electrocardiographic normalization. Oral calcium and vitamin-D preparation were prescribed on discharge. Future serial liver function tests and ionized calcium were advised. Later follow up with an endocrinologist and nephrologist for electrolytes imbalance will be recommended.
Figure 1: Serial ECG tracings showing; A-tracing: an initial ECG emergency on ICU admission showing widespread “U”-waves thorough ECG (red arrows), Tee-Pee sign (green arrows), Wavy double sign of hypocalcemia (Yasser’s sign; blue arrows), and evidence of RBBB (brown arrows), and sinus bradycardia of VR: 48 bpm. B-tracing: was taken within 3.18 hours of A-tracing and after starting the anti-ischemic measures, IVI of Potassium therapy, and three amps of IV atropine. It nearly showed the same of A-tracing but with marked sinus bradycardia with VR; 36 bpm. C-tracing: was taken within 9.33 hours of A-tracing and immediately after 2 amp of IV calcium therapy showing nearly normalization of all above ECG findings but with still evidence of RBBB (brown arrows) and VR: 68 bpm.
Figure 2: Serial ECG tracings showing; A-tracing: was taken within 11.30 hours of the last improvement showing the above widespread “U”-waves thorough ECG (red arrows), Wavy double sign of hypocalcemia (Yasser’s sign; blue arrows), and evidence of RBBB (brown arrows), and sinus bradycardia of VR: 44 bpm. B-tracing: was taken within 3.18 hours of A-tracing and after 2 amp of IV calcium therapy showing nearly normalization of all above ECG findings but with still evidence of RBBB (brown arrows) and VR: 74 bpm.
DISCUSSION
• Overview: A middle-aged male car-painter patient presented to the emergency department with atypical severe twisting chest pain, hypocalcemia, hypokalemia, and hypernatremia.
• The primary objective for my case study was the presence of anginal chest pain, bradycardia, hypocalcemia, hypokalemia, and hypernatremia.
• The secondary objective for my case study was the priority in the management of angina, bradycardia, severe hypocalcemia, severe hypokalemia, and mild hypernatremia.
• The twisting chest pain and its limited disappearance immediately after Calcium gluconate injection indicate the pain may be named as “chest tetany”. The chest pain didn’t relive after O2, anti-ischemic medications, and even after pethidine analgesia.
• The dramatic reversal of Camel-hump T-wave, Tee-Pee sign, Wavy double sign of hypocalcemia (Yasser’s sign) after calcium gluconate injection interpret that these signs were due to hypocalcemia.
• Despite hypokalemia-inducing Camel-hump T-wave was mentioned in the above literature as a cause, but it was so far here.
• Still present evidence of right bundle branch block give a possibility for non-pathological normal variant RBBB.
• The negative troponin test with non-conclusive ECG changes for ischemic heart disease (IHD), and normal echocardiography will quietly exclude the presence of IHD.
• Non-atropine bradycardia response is an indicator that the management of the cause of bradycardia sometimes is essential e.g. hypocalcemia in the current case. The etiology of the combination of hypocalcemia, hypokalemia, and hypernatremia in the current case is unknown. car-paint toxicity was the possible cause.
• Primary aldosteronism (Conn's syndrome) was the main differential diagnosis.
• I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near comparison.
• Study questions here; How did you manage the current case? What are the possible causes of the ECG changes?.
LIMITATIONS OF THE STUDY:
Because of it was a single case study, consideration of bias or missed cases was excluded. But, regards the current case and hypokalemic-induced Camel-hump T-Wave literature, the author thinks that the link between hypokalemia and Camel-hump T-Wave is controversial. Widening the research at this point will be advised. There was no longer a follow-up. Placebo is not considered in the study.
RECOMMENDATIONS
It is recommended to widening the research in clearing the presence of Camel-hump T-Wave, Tee-Pee sign, and Wavy double sign (Yasser’s sign) in hypocalcemia.
CONCLUSIONS
• The dramatic disappearance of Camel-hump T-Wave, Tee-Pee sign, Wavy double sign of hypocalcemia (Yasser’s sign), and bradycardia means that all these signs and finding were lonely due to severe hypocalcemia.
• Despite, it was a single case report, the author thinks that the study for a similar case report series or research will be recommended for support these results as possible.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENT
I wish to thank the nurses of the critical care unit in Fraskour Central Hospital who make extra-ECG copies for helping me.
REFERENCES
- Soar J, Deakin CD, Nolan JP, Abbas G, Alfonzo A, et al. (2010). European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 81(10):1400–33.
- Ed Burns. (2020). T wave. Available from: https://litfl.com/t-wave-ecg-library/ (Accessed: April 11, 2020).
- Abbott JA, Cheitlin MD. (1979). The Nonspecific Camel-Hump Sign. JAMA. 235(4):413–14.
- Lepeschkin E, Surawicz B. (1952). The measurement of the Q-T interval of the electrocardiogram. Circulation. 6(3):378-388.
- Dusky BMR. (2001). ECG Abnormalities Associated With Hypocalcemia. Chest. 119(2):668–669.
- Elsayd YMH. (2019). Wavy Triple an Electrocardiographic Sign (Yasser Sign) in Hypocalcemia. A Novel Diagnostic Sign; Retrospective Observational Study. EC Emergency Medicine and Critical Care (ECEC). 3(2):1-2. Available from: https://www.ecronicon.com/ecec/volume3-issue12.php. (Accessed: Nov 6, 2019).
- Johri AM, Baranchuk A, Simps on CS, Abdollah H, Redfearn DP. (2009). ECG Manifestations of Multiple Electrolyte Imbalance: Peaked T Wave to P Wave (“Tee-Pee Sign”). Ann Noninvasive Electrocardiol. 9(4):211-214.
Copyright: Elsayed YMH. ©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Elsayed YMH (2020). Hypocalcemia-induced Camel-hump T-wave, Tee-Pee sign, and bradycardia in a car-painter of a complexed dilemma: A case report. Cardiac 2(1):07.
 Abstract
Abstract  PDF
PDF