Past Issues
Six Minutes-Walk Test and Respiratory Function Tests Predict Complications and Mortality in Coronary Artery Bypass Grafting?
Mariana Graça Gutierrez1*, Iracema Ioco Kikuchi Umeda2, Lucas Mellaci Bergamascki3, Marília Amorim Souza Leão4
1Department of Physical Therapy, Dante Pazzanese of Cardiology Institute, SP, Brazil 2Department of Physical Therapy, University of São Paulo, SP, Brazil 3Faculty of Medical Sciences of Santa Casa deSão Paulo, SP, Brazil 4Faculty of Medical Sciences of Santa Casa de São Paulo, SP, Brazil
*Corresponding Author: Mariana Graça Gutierrez, Department of Physical Therapy, Dante Pazzanese of Cardiology Institute, 500 - Vila Mariana, Sao Paulo 04012-909, Brazil.
Received: October 31, 2019 Published: November 17, 2019
ABSTRACT
Objective: To disclose the relationships between clinical characteristics, six minute walk test, spirometry and inspiratory muscle strength with possible complications of coronary artery bypass grafting.
Method: Longitudinal observational studies with patients who will perform elective of coronary artery bypass grafting at the cardiology Hospital. Were included clinically stable patients of both sexes and older than 18 years old. The data collection was divided into preoperative, intraoperative and postoperative period. For quantitative variables was used the Student's t-test or the Mann-Whitney test. The verification of the association between categorical variables was used the Fisher or Chi-square test, and the Odds ratio estimate was calculated. The level of significance adopted was 5%.
Results: In the study, 52 patients who performed the surgery, 51.92% had some type of complication or died. Perfusion time high was predictors of hospital complications and mortality (p=0.05), as well a EuroScore above 2 (p=0.038), smoking or ex-smoking (p=0.04), low values of forced expiratory volume in the first second (p=0.035) and forced vital capacity (p=0.0001), high body mass index (p=0.01), and low values of inspiratory muscle strength (p=0.01).
Conclusion: Low values of forced expiratory volume in the first second, forced vital capacity and inspiratory muscle strength were predictive of complications and mortality in coronary artery bypass grafting. The six minute walk test wasn’t a predictor.
Keywords: 6-minute walk test, Coronary artery bypass, Spirometry, Maximal respiratory pressures.
INTRODUCTION
In the last decades, the frequency of surgical procedures has been increasing, especially coronary artery bypass grafting (CABG) [1]. CABG is considered one of the treatment options to alleviate symptoms, improve quality of life and decrease mortality in patients with coronary artery disease (CAD). In individuals older than 70 years is estimated that 70% of the CAD incidence is submitted to CABG [2]. In addition, in 2012 in Brazil, more than 102.000 cardiac surgeries were performed, demonstrating a severe public health problem [3]. The surgical procedure is considered of high complexity, affecting functional capacity and lung function. The need for sternotomy, capture of the internal thoracic artery graft [4], pleurotomy for insertion of the drains [5], and the use of extracorporeal circulation (EC) [6], lead to deleterious effects on pulmonary function. In addition, the procedure can lead to neurological, renal and cardiac complications [7], reduced functional capacity [8] and lead to death [6].
It is known that CABG leads to postoperative pulmonary complications, but it is still uncertain whether functional and pulmonary conditions prior to the surgical procedure have a significant impact on the incidence of complications and intra-hospital mortality. To assess functional capacity, the 6-minute walk test (6MWT) in the cardiopathy has been shown to be a good predictor of cardiovascular events. It is a method that is simple, safe, reproducible and easy to apply. According to the usual scientific literature, the 6MWT was considered a independent prognostic marker of mortality in patients with heart failure (HF) [9]. Regarding pulmonary-respiratory evaluation, the use of manovacuometry aims to identify changes in respiratory muscle strength and respiratory muscle training has already been shown to reduce the incidence of complications in the postoperative period of CABG [10]. Spirometry can also be used to assess lung function and aims to identify changes in volumes and capacities commonly present in the postoperative period, since the surgical procedure may generate a restrictive pattern related to the reduction of pulmonary functional residual capacity (FRC) [11]. Due to the features of the surgical procedure, intra- and postoperative complications are present, and some available mortality scores and studies associate the clinical and operative characteristics with the increased incidence of complications and death. However, there is still a gap regarding the usefulness of functional and respiratory evaluation to assist in the identification and prevention of possible complications in order to guide a more appropriate management in order to prevent significant functional losses and complications in order to reduce the time of hospitalization. Thus, this study goal was to verify the relationship between clinical characteristics, functional capacity, spirometric values and respiratory muscle strength with possible intra and postoperative complications of CABG.
METHODS
Study design
A longitudinal observational study with patients enrolled in the outpatient cardiac elective coronary artery bypass surgery from February to July 2018 in a tertiary public hospital specialized in cardiovascular care. Approved by the Research Ethics Committee of the Dante Pazzanese Institute of Cardiology (DPIC) with CAAE: 73637317.7.0000.5462 and was carried out following the guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) for observational studies [12]. The patients were evaluated in the period of hospital admission for CABG and received follow-up in the pre and postoperative period (intensive care unit and ward) until hospital discharge.
Eligibility criteria
We included clinically stable patients of both sexes over the age of 18, who were literate and referred for elective coronary artery bypass surgery through the specialty outpatient clinic, who signed the Informed Consent Form (ICF). Patients with psychiatric or neurocognitive conditions who were unable to obtain reliable clinical data and / or musculoskeletal problems that interfered walk test evaluations were excluded from the study.
Sample
Ninety-seven patients met the eligibility criteria and signed the ICF. The sample was calculated from the study by Riedi et al. [13] using as main outcome the inspiratory muscle strength (IMS), whose standard deviation was found to be 50 cmH2O15. Assuming this standard deviation, for a significant difference of 50 cm H2O with 80% test power and 5% alpha (error type 1) performed by the Mann Whitney test, the target sample size was 40 subjects.
Data collection and following
After receiving the medical instructions to schedule the surgery, the patients were screened and referred to the multiprofessional clinic, where they were guided about the research and after signing the ICF, were screened according to the hospitalization forecast.
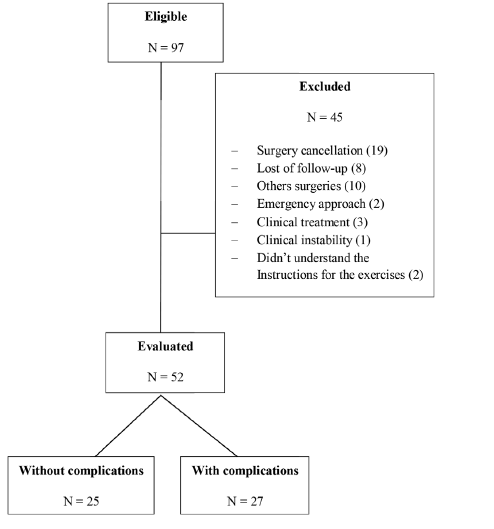
A specific evaluation form was used to collect the variables of interest. This evaluation was divided into three stages: preoperative, intraoperative and postoperative periods. In Figure 1, it is possible to observe the flowchart of the data collection’s steps.
Figure 1: Flowchart: Data collection steps.
Preoperative stage
In this stage, the clinical features related to the preoperative condition of the patients, collected from the chart were identified: sex, age, weight, height, date of hospital admission, personal history, European System for Cardiac Operative Risk Evaluation (EuroScore) [14], and left ventricular ejection fraction (LVEF) according to the echocardiogram, classified by the Simpson method [15].
An evaluation of the physical capacity determined by the 6MWT, evaluation of pulmonary function by spirometry and respiratory muscle strength were performed by means of the manovacuometry.
It was considered the period in which the patient entered the surgical center until discharge to the immediate postoperative intensive care unit (ICU). Data about anoxia time, extracorporeal circulation time, and intraoperative complications were collected from the charts.
Postoperative stage
Data were collected from medical records concerning immediate and mediate postoperative complications, intercorrences during the time the individual remained in the postoperative ICU and in the postoperative ward, respectively.
The following were considered as complications in the ICU and ward: death, stroke, delirium, respiratory failure, increased bleeding, cardiorespiratory arrest, arrhythmias, shock and surgical wound infection.
6-minute walk test
The test was performed following the American Thoracic Society Guidelines [16] in a 30 meter corridor with flat surface; the patient was instructed to walk as fast as he could without running. If there was any sign or symptom of exertion intolerance, the patient could stop in the hallway and lean/sat in the chair. The test was performed only once.
At the beginning of the test were evaluated: blood pressure (BP), measured with sphygmomanometer (Premium®), heart rate (HR) and peripheral oxygen saturation (SpO2) with pulse oximeter (Contec Medical Systems®) and perceived exertion using the adapted Borg Scale [16].
At the end of the walk the distance traveled was measured, and the HR, SpO2 and the adapted Borg scale were repeated at 6 minutes and at 8 minutes of recovery. The examination was performed under the guidance of the same physiotherapist, who did not go along with the patient during the walk [16].
Pulmonary function test
Pulmonary function testing (PFT) was performed using the spirometer (Easy One Plus Portable Spirometer Machine®-ndd Medical Technologies). The maneuver performed was forced vital capacity (FVC) with the patient in the seated position and using a nasal clip, and it was performed three times. The patient was instructed to breathe at the tidal volume level (TV), followed by a maximal inspiration from the FRC, then exhaled air to the residual volume (RV), ending with deep inspiration until lung total capacity (LTC) [17]. The values were predicted by age, height and sex according to the equation of Pereira et al. [18]. FVC, forced expiratory volume in the first second (FEV1) and the ratio of forced expiratory volume in the first second to forced vital capacity (FEV1/FVC) were evaluated.
Respiratory muscle strength
Measurement of ventilatory muscle strength was performed with the analogical manovacuometer (Comercial Médica®) with the individuals seated, the trunk at a 90º angle to the thighs and the airway occluded by a nasal clip. The patient was instructed to perform respiration at TV level, followed by an expiration to RV and a deep inspiration up to LTC for maximal inspiratory pressure (MIP) value [19,20].
The values obtained were MIP, a measure that predicts static inspiratory muscle strength, with a rest interval of 1 minute. A total of five maneuvers were performed, of which three were accepted and at least two of them should present difference values less than 10% of the highest value. To determine the predictive values of each patient, according to age and sex, we used the equations of Neder et al. [21].
EuroScore
EuroScore was calculated according to the 17-item model that assesses patient-related risk factors and cardiac and surgical factors by chart analysis. The score is divided into low mortality risk with score from 0 to 2, moderate risk from 3 to 5 and high risk with scores above 6 [22].
Patient risk factors assess age, sex, presence of chronic obstructive pulmonary disease, extracardiac arteriopathy, neurological dysfunction, previous cardiac surgery, active endocarditis, critical preoperative status, and serum creatinine values [22].
Cardiac risk factors evaluate the presence of unstable angina, left ventricular dysfunction, recent acute myocardial infarction, and the presence of pulmonary hypertension. Moreover, the surgical factors assess the presence of emergency procedure, other surgeries besides CABG, thoracic aortic surgery and the presence of post-infarction ventricular septal defect [22].
Statistical method
Quantitative variables were expressed as mean and standard deviation, and qualitative variables were expressed by absolute frequency and percentage. To evaluate the normal distribution of the data the Komogorov-Smirnov test was used. For the comparison between the groups for the quantitative variables the Student's t-test or the Mann-Whitney test was used. Verification of the association between categorical variables was performed using Fisher's exact test or Chi-square test, and the estimated odds ratio (OR) was calculated. The significance level was 5%.
Results
Participants
A total of 97 participants were eligible for the study from February to July 2018, who were admitted to the outpatient clinic for CABG, with 45 excluded and 52 participants remaining for evaluation, which 27 presented some type of complication or died and 25 participants without complications, as shown in Figure 2.
Figure 2: Eligibility’s flowchart.
Characterization of the sample
The characteristics of the participants are shown in Table 1. It can be observed that the sample was divided according to the time of the manifestation of the complications.
Table 1: Characteristics of participants with and without complications (n=52).
| Variables | Table (n = 52) | General Complications | Complications in the ICU | Complications in the Ward | Deaths | ||||
| Without Complications(n=25) | Complications(n=27) | Without Complications(n=37) | Complications(n=15) | Without Complications(n=34) | Complications(n=14) | Survivors(n=48) | Deaths(n=4) | ||
| Age (Years) | 62.6±9.6 | 61.3±8.6 | 64.0±10.6 | 62.1±9.4 | 64.0±10.4 | 62.2±9.0 | 62.0±12.1 | 62.2±9.9 | 68.2±1.7 |
| BMI(Kg/m2) | 28.7±4.8 | 27.5±4.8 | 29.8±4.6 | 28.1±4.5 | 30.1±5.3 | 27.6±4.6 | 29.6±4.0 | 28.2±4.5 | 24.9±4.4* |
| Male | 78.8(41) | 84.0(21) | 74.1(20) | 78.3(29) | 80.0(12) | 88.2(30) | 57.1(8)* | 79.1(n=38) | 75.0(3) |
| Female | 21.2(11) | 16.0(4) | 25.9(7) | 21.6(8) | 20.0(3) | 11.8(4) | 42.9(6) | 20.8(n=10) | 25.0(1) |
| Antecedentes | |||||||||
| Non- Smokers | 46.2(24) | 52.0(13) | 40.7(11) | 54.0(20) | 26.6(4) | 47.0(16) | 50.0(7) | 47.9(n=23) | 25.0(1) |
| Former Smokers | 48.1(25) | 48.0(12) | 48.1(13) | 43.2(16) | 60.0(9)* | 50.0(17) | 35.7(5) | 45.8(n=22) | 75.0(3) |
| Active Smokers | 5.8(3) | 0.0(0) | 11.1(3) | 2.7(1) | 13.3(2)* | 2.9(1) | 14.3(2) | 6.2(n=3) | 0.0(0) |
| Non-dialytic CRF | 13.5(7) | 4.0(1) | 22.2(6) | 10.8(4) | 20.0(3) | 8.8(3) | 21.4(3) | 12.5(n=6) | 25.0(1) |
| Systemic Artial Hypertension | 88.5(46) | 84.0(21) | 92.6(25) | 86.4(32) | 93.3(14) | 88.2(30) | 92.9(13) | 89.5(n=43) | 75.0(3) |
| Acute Myocardial Infarction Previous | 46.2(24) | 40.0(10) | 51.9(14) | 40.5(15) | 60.9(9) | 47.0(16) | 50.0(7) | 12.5(n=6) | 25.0(1) |
| Stroke Previous | 13.5(7) | 12.0(3) | 14.8(4) | 13.5(5) | 13.3(2)1 | 11.8(4) | 14.3(2) | 12.5(n=6) | 25.0(1) |
| Diabetes Mellitus Type 2 | 53.8(28) | 56.0(14) | 51.9(14) | 54.0(20) | 53.3(8) | 50.0(7) | 57.1(8) | 52.0(n=25) | 75.0(3) |
| Dyslipidemia | 75.0(39) | 76.0(19) | 74.1(20) | 78.3(29) | 66.7(10) | 73.5(25) | 85.7(12) | 77.0(n=37) | 50.0(2) |
| Quarter of LVEF | |||||||||
| LVEF Preserved (>50%) | 75.0 (39) | 64.0 (16) | 85.2 (23) | 70.3 (26) | 86.7 (13) | 67.6 (23) | 85.7 (12) | 72.9 (n=35) | 100.0 (4) |
| LVEF Reduced (<50%) | 19.2 (10) | 28.0 (7) | 11.1 (3) | 24.3 (9) | 6.7 (1) | 23.5 (8) | 14.3 (2) | 20.8 (n=10) | 0.0 (0) |
| LVEF Serious (<35%) | 5.8 (3) | 8.0 (2) | 3.7 (1) | 5.41 (2) | 6.7 (1) | 8.8 (3) | 0.0 (0) | 6.25 (n=3) | 0.0 (0) |
| EuroSCORE | |||||||||
| Low Risk (0-2) | 32.7 (17) | 48.0 (12) | 18.5 (5) | 40.5 (15) | 13.3 (2) | 41.2 (14) | 21.4 (3) | 35.4 (n=17) | 0.0 (0) |
| Moderate Risk (3-5) | 34.6 (18) | 28.0 (7) | 40.7 (11)* | 32.4 (12) | 40.0 (6) | 32.4 (11) | 35.7 (5) | 33.3 (n=16) | 50.0 (2) |
| High Risk(>6) | 32.7 (17) | 24.0 (6) | 40.7 (11) * | 27.0 (10) | 46.7 (7) | 26.5 (9) | 42.9 (6) | 31.2 (15) | 50.0 (2) |
| Legend: BMI= Body Mass Index; CRF = Chronic Renal Failure; Kg =Kilogram; LVEF= Left Ventricular Ejection Fraction; M2= Square Meters; %=Percentage. Note: values presented in mean ± SD; * = Significance p>0.005. | |||||||||
About three-quarters of the analyzed sample presented a preserved LVEF, ie, LVEF >50%, and mortality risk values in cardiac surgery according to EuroScore were similar in their subdivisions, demonstrating itself as a homogeneous group.It is observed that the participants of this study have an average age above 60 years and about 78.8% of the participants were male. Participants were classified as overweight according to body mass index (BMI) data based on the World Health Organization (WHO) classification and the Brazilian Association for the Study of Obesity and Metabolic Syndrome [23]. In addition, the most prevalent personal antecedents were: ex-smoking, stroke, type 2 diabetes mellitus (DM), dyslipidemia and systemic arterial hypertension with 88.5% (n=46).
Table 2 shows the manovacuometry data of the study participants. The values found for MIP were, on average, 60% of the predicted. In spirometry, it was possible to observe a mean FEV1/FVC ratio above 70% of the predicted and mean FVC above or equal 80% of the predicted, which values are classified as normal [18].
Table 2: Evaluation of inspiratory, muscle strength and spirometric values of study participants (n=52).
| Pulmonary variables | Total (n=52) | General complications | Complications in the ICU | Complications in the Ward | Deaths | ||||
| Without Complications (n=25) | Complications (N=27) |
without Complications (n=37) |
Complications (N=15) | Without Complications (n=34) | Complications (N=14) | Survivors (N=48) | Deaths (N=4) | ||
| Respiratory muscle strength MIP (mmhg) | 65.1 ± 27.1 | 69.9±25.2 | 60.7±28.7 | 66.0±27.3 | 63.0±27.5 | 69.4±24.1 | 56.8±28.9 | 65.7±26.0 | 58.0±43.3 |
| % Expected MIP | 61.0±24.0 | 66.1±20.4 | 56.0±26.4 | 63.8±23.4 | 54.6±24.9 | 65.7±20.5 | 59.0±27.1 | 63.7±22.5 | 29.7±19.6* |
| Spirometry Values FEVI (L) | 2.1±0.8 | 2.2±0.9 | 2.0±0.8 | 2.0±0.9 | 2.2±0.8 | 2.3±0.9 | 1.6±0.7* | 2.1±0.9 | 1.9±0.9 |
| % Predicted FEVI | 69.0±22.0 | 71.7±20.5 | 66.9±24.3 | 68.8±22.3 | 70.1±23.9 | 73.8±21.3 | 61.0±24.6 | 70.0±22.8 | 60.0±18.1 |
| FVC (L) | 3.1±1.0 | 3.5±0.9 | 2.7±0.9* | 3.2±1.1 | 2.9±0.9 | 3.5±0.9 | 2.4±0.9* | 3.21±1.0 | 2.0±1.1 |
| % Predicted FVC | 80.0±21.0 | 90.0±18.8 | 72.4±20.9* | 82.7±22.1 | 75.7±20.2 | 88.0±18.3 | 69.5±20.3* | 82.5±20.6 | 59.5±25.7 |
| FEVI/FVC | 0.6±0.3 | 0.7±0.5 | 0.6±0.1 | 0.7±0.4 | 0.6±0.1 | 0.7±0.4 | 0.6±0.1 | 0.7±0.3 | 0.6±0.2 |
| % Predicted FEVI/FVC | 85.0±18.0 | 81.7±18.2 | 88.4±19.0 | 84.7±17.3 | 86.6±22.5 | 85.4±18.1 | 86.9±17.7 | 85.8±17.8 | 78.2±30.5 |
| Legend: FEVI = forced expiratory volume in the first second; FVC =forced vital Capacity; L=liters; MIP=maximal inspiratory pressure; mmHg = millimeters of mercury;% =percentage. NOTE: Values presented in mean ± SD; *=significance p>0.05. | |||||||||
Table 3 presents data from the six-minute walk test with mean distance travelled above 300 meters, indicative of a mean above 70% of that predicted for this population [16]. During the surgical procedure, data on perfusion time, anoxia time and complications were analyzed. The perfusion time was on average 88.75 ± 27.46 minutes and the anoxia time was 60.37 ± 16.87 minutes, both considered as a normal duration for the procedure [24].
Table 3: Evaluation of functional capacity by the 6MWT of the participants analyzed in the study (n=52).
| Variables of functional capacity | Total (n=52) | General complications | Complications in the ICU | Complications in the ward | Deaths | ||||
|
Without complications(n=25) |
Complications(n=27) | Without complications (n=37) | Complications (n=15) | Without complications (n=34) | Complications (n=14) | Survivors (n=48) | Deaths (n=4) | ||
| 6mwtDistance (m) | 357.1±104.7 | 373.8±102.0 | 341.5±106.7 | 355.3±105.1 | 361.4±107.4 | 378.2±101.6 | 320.3±97.9 | 361.4±103.0 | 305.5±128.3 |
| % predicted of distance | 72.1±22.8 | 72.4±21.3 | 73.3±24.3 | 71.0±22.1 | 77.8±24.6 | 74.6±23.8 | 67.7±22.4 | 72.623.4 | 77.0±9.4 |
| Legend: m=meters; %= percentage. Note: Value presented in mean ± SD; *= Significance p >0.05. | |||||||||
General complications
The general complications were subdivided into complications in the ICU, in the ward and deaths. According to the analyzed sample, 51.9% (n=27) of the participants presented some type of complication. The perfusion time 95.96 ± 29.71 minutes (p=0.054) was a predictor of complications of CABG. EuroScore was also considered a predictor of complications since 81.5% of the volunteers who complicated presented values above 2 in their score (p=0.038).
Table 4 shows the OR values for individuals with EuroScore above 2 on the scale (moderate risk) and non-dialytic chronic renal failure (CRF) were not considered a predictors of complications in this sample, but increase the chances of developing complications.
Table 4: Odds ratio (OR) statistical data.
| Variables | General complications | Complications in the ICU | Complications in the ward | Deaths |
| EuroScore above 2 | 4,06 | 4,43 | 2,56 | Incalculable |
| Non-dialytic CRF | 6,85 | 2,06 | 2,81 | 2,33 |
| Dyslipidemia | 0,90 | 0,55 | 2,16 | 0,29 |
| Diabetes Mellitus type 2 | 0,84 | 0,97 | 1,33 | 2,76 |
| Legend: CRF = chronic renal failure; EuroScore = European System for Cardiac Operative Risk Evaluation. | ||||
Complications and death in the ICU
The general sample’s ICU length of stay was on average 3.29 ± 2.09 days and of the participants who presented complications or died, 28.8% (n=15) were in the ICU. The assessed complications were: arrhythmia (atrial fibrillation and atrioventricular block) in 7.7% of the participants; 5.8% presented acute respiratory failure; 1.9% with stroke and 1.9% with delirium; 1.9% with cardiorespiratory arrest and 1.9% with shock; and 7.7% died.
Smoking was identified as a predictor of complications and death in the ICU. A sample of 73.3% of the participants were former smokers or active smokers verified by a linear association (p=0.04).
Complications in the ward
Of the 27 participants who had complications, 29.2% (n=14) were in the ward. It was possible to observe that 9 had respiratory complications, 2 had complications of the surgical wound, 1 had cardiovascular complications and 2 had associated complications. It was observed that the male sex (57.1%) was a predictor of complications in the ward (p=0.04), but we could not find any association between the complications related to sex.
The spirometric values of the patients who had complications were lower when compared to the values of the patients without complications and it was possible to observe that FEV1 (p=0.035), FVC (p=0.0001) and percentage of predicted FVC (p=0.009) had a significant association with complications in the ward. It was also observed that participants with complications had, prior to surgery, a mild restrictive pattern disorder. The OR demonstrated that the presence of dyslipidemia may also increase the chances of developing complications.
Deaths
All of the participants who died were in the ICU and presented a high BMI, indicative of obesity grade 1, which was considered a predictor of mortality in the sample evaluated (p=0.01). In addition, the predicted percentage of MIP prior to surgery was also considered a predictor of mortality (p=0.01), as these participants presented MIP on average 29.7% of predicted, a value that is 70% below the expected for a population without pulmonary disturbances. OR analysis has shown that the presence of diabetes can increase the chances of death.
DISCUSSION
The present study identified as predictors of complications and in-hospital mortality, surgical variables such as perfusion time, EuroScore clinical variables over 2, smokers or former smokers, BMI, and variables of pulmonary-respiratory assessment preoperative spirometric values (FEV 1 and FVC) below the predicted and reduced values of MIP. The 6MWT was not considered a predictor of complications and mortality in patients undergoing elective CABG, but the literature points out its importance and effectiveness in the evaluation of patients with HF.
High BMI has a role that increases the chances of complications in the postoperative period, Dordetto et al. [25] have shown that overweight and obesity are indicators of surgical failure due to the pathogenesis of obesity that elevates inflammatory markers and further exacerbates inflammatory response when associated with DM type 2 [5].
Araújo et al. [26] analyzed the repercussion of overweight and obesity in the postoperative period of CABG and identified that the obese patients had more grafts in the CABG and had a higher mortality rate, in addition, patients classified as overweight presented longer surgery and CE time, greater risk of developing neurological events and a higher rate of cardiovascular complications and length of hospital stay. In our study, overweight was related to postoperative complications and grade 1 obesity was considered a predictor of ICU mortality.
EuroScore is a simple and objective predictor of operative mortality, but Campagnussi et al. [14] demonstrated that a sample of 100 individuals is required to be universally applicable. In our study, although the EuroScore values were close between their subdivisions, the incidence of death was small, not sharing results given by the score. It was observed that individuals with a moderate risk to high risk classification had a higher chance of developing complications during hospitalization and 2.56 times more likely to develop complications in the ward, and that there was no association with in-hospital mortality.
Smoking and quit smoking were also predictors of postoperative complications of CABG according to our results. A systematic review by Critcheley et al. [27] with a final analysis of 20 studies suggests that cessation of smoking reduces the risk of mortality after surgical interventions. Cigarette smoking results in an increased oxygen consumption, concomitantly with a decreased oxygen supply by the levels of carboxyhemoglobin and elevation of coronary vascular resistance, leading to changes in the cardiovascular system such as heart rate, stimulation of chemoreceptors and reduction of pulmonary functional residual capacity [28].
Perfusion time was also a predictor of complications. In our study it was 88.75 ± 27.46 minutes. It is not observed in the scientific literature an ideal time for CE time, which is known to be related to the time of each surgery [24]. The literature also indicates that longer CE time may contribute to congestion, injury of the pulmonary vascular endothelium and decrease of respiratory muscle strength, leading to a longer time of postoperative ventilatory assistance [29].
In the study performed by Torrati et al. [30], 83 patients underwent cardiac surgery of CABG, valvular surgery and combined surgery. The sample was divided into two groups, one group with CE time less than 85 minutes (n=44) and the other with time greater than 85 minutes (n=39), both groups had the same complications with similar incidences in both the groups. It was different from our study, where CE time was considered a predictor of complication, but in the study by Torrati et al. not only one type of surgery was selected, but also there was approach for heart valve replacement surgery, with a longer CE time than 85 minutes.
Spirometric values are usually used to verify restrictive and obstructive disorders in order to identify the presence of asthma or chronic obstructive pulmonary disease in the population, but it is not routine to perform it in the preoperative period. In our study, in the ward, pulmonary variables were predictive of complications with a predominance of mild restrictive disorder, with FVC between 60% and 80%. Patients with spirometric values below normal are more likely to develop postoperative complications of CABG, and therefore, this evaluation should be instituted as an auxiliary tool in the preoperative evaluation in order to guide pre and postoperative prophylactic procedures.
Hulzebos et al. [10] performed respiratory muscle training in preoperative CABG patients in order to prevent postoperative pulmonary complications. It was identified that the training reduced the rate of postoperative complications and hospitalization time in patients at high risk of developing pulmonary complications, ie, patients with spirometric values and respiratory muscle strength below normality.
Inspiratory muscle strength is still underused in the routine evaluation of these patients. This data may demonstrate the need for respiratory muscle training to promote better respiratory conditions for the patients who will perform the surgical procedure. Our population had an average of 29.7% of predicted inspiratory muscle strength, which may be highly related to postoperative complications.
Morsch et al. [31] evaluated the preoperative respiratory muscle strength and found an average MIP similar to the values found in our study sample. Moreover, there was a significant difference in MIP in the postoperative period, when compared with preoperative values. In another study, Mendes and Borghi-Silva et al. [32] observed that reduced respiratory muscle strength is related to worsening pulmonary function, leading to a higher incidence of postoperative pulmonary complications.
In the evaluation of functional capacity, the 6MWT was not considered a predictor of complications and mortality in our population, despite being predictive of hospitalization and mortality in patients with HF. According to Rubim et al. [9] the 6MWT 'has been shown to be reliable for evaluation and to predict mortality in a potent and independent way in patients with HF, whose degree of left ventricular dysfunction is related to a worse prognosis of the disease. In addition, it was considered to be of intense activity for these patients, not being representative of activities of daily living. In preevaluation of patients for the cardiac transplant queue, the 6MWT 'showed a correlation between the distance traveled, perceived exertion and heart rate when compared to surviving patients and those who died [33].
Another important finding was the incidence of non-dialytic CRF in the preoperative period. Although it was not associated with complications in our sample, it was possible to analyze by the OR that patients with CRF are 6.85 times more likely to develop postoperative complications, 2.81 times more likely to complicate in the ward and 2.33 times more chances of dying in the ICU. Barbosa et al. [34] demonstrated that patients with chronic kidney disease undergoing CABG present a high risk of complications and in-hospital mortality in the postoperative period, besides the progression of the disease to the need for dialysis therapy. Furthermore, complications and mortality were associated with female sex, smoking, diabetes mellitus, presence of peripheral and/or carotid vascular disease.
Limitations
We had a considerable loss of patients due to cancellation of the surgery, and others types of approach to CABG that were concomitant, such as valve replacement and aneurysm repair. Futhermore, high-risk patients or those who required emergency surgery, which could impact on the results, were not evaluated. For the future, there is a need for new observational studies that include this type of patients.
CONCLUSION
The present study identified as predictors of complications and in-hospital mortality the preoperative spirometric values below predicted (FEV1 and FVC) and reduced values of inspiratory muscle strength; the six-minute walk test was not a predictor.
Acknowledgments
To all the collaborators at work.
Conflict of Interest
The authors report no relationships that could be construed as a conflict of interest.
REFERENCES
- Sobrinho MT, Guirado GN, Silva MA (2014) Preoperative therapy restores ventilatory parameters and reduces length of stay in patients undergoing myocardial revascularization. Rev Bras Cir Cardiovasc 29(2): 221-228.
- Cameron A, Davis KB, Green G, Schaff HV (1996) Coronary bypass surgery with internal-thoracic-artery grafts-effects on survival over a 15-year period. N Engl J Med 334(4): 216-219.
- Bocchi EA, Marrcondes-Barga FG, Bacal F, Ferraz AS, Albuquerque D, et al. (2012) Brazilian chronic heart failure guideline update. Arq Bras Cardiol 98(1 Suppl 1): 1-33.
- Vargas FS, Terra-Filho M, Hueb W, Teixeira RL, Cukier A, Light RW (1997) Pulmonary function after coronary artery bypass surgery. Respir Med 91(10): 629-633.
- Guizilini S, Gomes WJ, Faresin SM, Carvalho ACC, Jaramillo JI, et al. (2004) Effects of pleural drainage site insertion on pulmonary function after myocardial revascularization surgery. Rev Bras Cir Cardiovasc 19(1): 47-54.
- Conti VR (2001) pulmonary injury after cardiopulmonary bypass. Chest 119(1): 2-4.
- Strabelli TMV, Stolf NAG, Uip DE (2008) Practical use of a risk assessment model for complications after cardiac surgery. Arq Bras Cardiol 91(5): 342-347.
- Benvenuti SM, Patron E, Zanatta P, Polesel E, Palomba D (2014) Pre-existing cognitive status is associated with reduced behavioural functional capacity in patients 3 months after cardiac surgery: An extension study. Gen Hosp Phychiatry 36(4): 368-374.
- Rubim VSM, Neto CD, Romeo JLM, Montera MW (2006) Prognostic value of six-minute walk test in heart failure. Arq Bras Cardiol 86(2): 120-125.
- Hulzebos EHJ, Helders PJM, Favie NJ, Bie RA, Riviere AB, et al. (2006) Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG Surgery. JAMA 296(15): 1851-1857.
- Qaseem A, Snow V, Fitterman N, Hornbake ER, Lawrence VA, et al. (2006) Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing non-cardiothoracic surgery: A Guideline from the American College of Physicians. Ann Intern Med 144(8): 575-580.
- Malta M, Cardoso LO, Bastos FI, Magnanini MMF, Silva CMFP (2010) Strobe initiative: Subsidies for reporting observational studies. Rev Saude Publica 44(3): 559-565.
- Riedi C, Mora CTR, Driessen T, Coutinho MCG, Mayer DM, et al. (2010) Relationship of muscle strength behaviour with respiratory complications in cardiac surgery. Rev Bras Cir Cardiovasc 25(4): 500-505.
- Campagnucci VP, Pinto ANMS, Pereira WL, Chamlian EG, Gandra SMA, et al. (2008) Euro SCORE and patients undergoing coronary artery bypass grafting at Santa Casa de São Paulo. Rev Bras Cir Cardiovasc 23(2): 262-267.
- Folland ED, Parisi AF, Moynihan PF, Jones DR, Feldman CL, et al. (1979) Assessment of left ventricular ejection fraction and volumes by real-time, two-dimensional echocardiography: A comparison of cineangiographic and radionuclide techniques. Circulation 60(4): 760-766.
- American Thoracic Society (2002) ATS Statement: Guidelines for the six-minute walk test. Am J Respr Crit Care Med 166(1): 111-117.
- Costa D, Jamani M (2001) Bases fundamentais da espirometria. Rev bras fisioter 5(2): 95-102.
- Pereira CAC, Barreto SP, Simões JG, Pereira FWL, Gerstler JG, et al. (1992) Reference values for spirometry in a sample of the adult Brazilian population. J Pneumol 18: 10-22.
- Black LF, Hyatt RE (1969) Maximal respiratory pressures: Normal values and relationship to age and sex. Am Rev Respir Dis 99(5): 696-702.
- Souza RB (2002) Pressões respiratórias estáticas máximas. J Pneumol 28(3): 155-165.
- Neder JA, Andreoni S, Lerario MC, Nery LE (1999) Reference values for lung function tests. II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res 32(6): 719-727.
- Moraes F, Duarte C, Cardoso E, Tenório E, Pereira V, Lampreia D, et al. (2006) Evaluation of Euro SCORE as a predictor of mortality in coronary artery bypass grafting at the Heart Institute of Pernambuco. Rev Bras Cir Cardiovasc 21(1): 29-34.
Copyright: Gutierrez MG, et al. ©2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Gutierrez MG (2019). Six Minutes-Walk Test and Respiratory Function Tests Predict Complications and Mortality in Coronary Artery Bypass Grafting? Cardiac 1(1): 3.
 Abstract
Abstract  PDF
PDF.PNG)